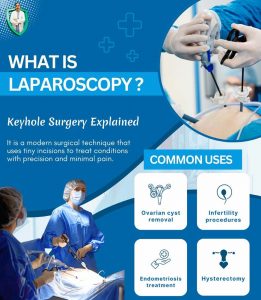
Laparoscopy in Women’s Health: Keyhole Surgery Explained
Nisha was having unexplained pelvic pain or infertility issues. I during my routine investigation prescribed laproscopy to her. She expressed her worry about a large scar from surgery. She was relieved when I explained that her condition could be treated using laparoscopy.
The technique, often called keyhole surgery, has transformed gynecology and is now one of the most preferred approaches in women’s health. Globally, minimally invasive surgery is expanding rapidly, with studies showing that over 70% of gynecological operations in leading centers are performed laparoscopically. In India too, demand has grown steadily as women look for safer, quicker, and less painful procedures.
 With years of experience in gynecology, I have seen how laparoscopy in women’s health transforms patient outcomes and offers safer, more effective treatment options. My experience in managing high-risk pregnancies, infertility, and gynecological surgery, I know how this approach can change outcomes for patients.
With years of experience in gynecology, I have seen how laparoscopy in women’s health transforms patient outcomes and offers safer, more effective treatment options. My experience in managing high-risk pregnancies, infertility, and gynecological surgery, I know how this approach can change outcomes for patients.
This article explains what laparoscopic surgery means, its diagnostic and therapeutic uses, the benefits and risks, and how it compares with open surgery.
Also Read:
- Recognising the Warning Signs of Ectopic Pregnancy Early
- Laparoscopy Recovery: Tips for Diet, Lifestyle, and Healing
Defining Laparoscopic Surgery in Women’s Health
Many women are unsure what a laparoscopic procedure actually involves. Defining laparoscopic surgery clearly helps reduce fear and prepares patients better for their treatment journey.
What Is Keyhole Surgery?
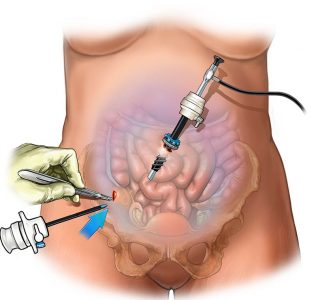
- Small incisions through which a laparoscope, a camera-equipped tube, is inserted
- Gas insufflation of the abdomen to create space for instruments
- Long, thin instruments used to perform precise surgical actions
- Smaller scars, speedier healing, and shorter admissions
 Keyhole operations are performed under general anesthesia, and patients are usually able to return home much earlier than with open surgery.
Keyhole operations are performed under general anesthesia, and patients are usually able to return home much earlier than with open surgery.
Patient Preparation Basics
- Fasting after midnight before surgery
- Reviewing and adjusting medications such as blood thinners before surgery
- Wearing loose clothing and removing jewelry on the day of surgery
- Arranging transport because of the after-effects of anesthesia
Understanding what is keyhole surgery and how patient preparation works is the first step in making women feel confident about their procedure.
Diagnostic Laparoscopy and Gynecological Operations
Diagnostic laparoscopy offers a clear view of the pelvic organs when non-invasive scans are not enough. It is widely used by gynecology and laparoscopic surgeons to identify underlying causes of symptoms.
 Diagnostic Applications
Diagnostic Applications
- Evaluation of chronic pelvic pain
- Identification of endometriosis or adhesions
- Biopsy and cancer staging
- Checking fallopian tubes and ovaries for structural problems
Unlike scans, diagnostic laparoscopy provides direct visualization of the uterus, ovaries, and fallopian tubes. This makes it an essential step in many gynecological operations where precision is needed.
Role of Gynecology and Laparoscopic Surgeons
- Specialists trained in minimally invasive surgery
- Use of advanced cameras for magnified views
- Ability to detect early disease changes
- Expertise in shifting from diagnostic to therapeutic treatment when required
Diagnostic laparoscopy in women’s health has become an essential tool in ensuring accurate diagnosis, reducing delays in treatment, and guiding safer surgical decisions.
Therapeutic Laparoscopy in Women’s Health
Beyond diagnosis, therapeutic laparoscopy allows surgeons to treat conditions during the same procedure. This dual approach avoids repeat surgeries and leads to better overall recovery.
 Common Gynecological Operations
Common Gynecological Operations
Laparoscopy is widely used in gynecology to treat common conditions. These procedures offer precise treatment through small incisions, reducing pain, recovery time, and the need for traditional open surgery.
- Removal of ovarian cysts
- Treatment of endometriosis
- Myomectomy for uterine fibroids
- Laparoscopic hysterectomy where necessary
Therapeutic laparoscopy is often chosen for women with complex conditions because of its precision and reduced impact on surrounding tissues.
Benefits of One-Step Diagnosis and Treatment
Laparoscopy allows both diagnosis and treatment in the same session. This approach avoids repeat surgeries, reduces patient stress, and helps women recover sooner with less disruption to daily life and responsibilities.
- Reduced need for multiple hospital visits
- Shorter anesthesia exposure
- Faster return to routine life
- Lower overall treatment costs
This ability to move seamlessly from diagnostic laparoscopy to therapeutic laparoscopy within the same session is one of the greatest advantages of minimally invasive surgery in modern gynecology.
Benefits and Risks of Laparoscopy vs Open Surgery
Every woman wants to know whether laparoscopy is safe and how it compares with traditional open surgery. The choice often depends on the patient’s health, the complexity of the procedure, and the surgeon’s expertise.
Benefits of Laparoscopy
Women often ask why laparoscopy is preferred over traditional surgery. Its minimally invasive approach offers several advantages, from smaller scars to faster healing, making it one of the safest options in modern gynecology.
- Shorter hospital stay, sometimes outpatient
- Smaller scars and better cosmetic outcomes
- Less pain and faster return to daily life
- Reduced infection risk
 Potential Risks and Complications
Potential Risks and Complications
Even with its advantages, laparoscopy carries some risks. Understanding possible complications helps women make safer, informed surgical decisions.
- Rare trocar injuries to vessels or organs
- Anesthesia-related risks
- Gas-related discomfort such as shoulder pain
- Possibility of conversion to open surgery in complex cases
Laparoscopy vs Open Surgery at a Glance
When choosing surgery, women often compare laparoscopy with traditional open surgery. Both have unique advantages and limitations. A clear comparison highlights why keyhole operations are increasingly favored for safety, recovery, and overall patient experience in gynecology.
- Open procedures mean wider scars, higher pain levels, and a slower return to normal activities.
- Laparoscopy: small incisions, faster healing, minimal scarring
Women considering abdominal and pelvic surgery should discuss with their gynecology and laparoscopic surgeons to evaluate if a laparoscopic procedure is right for them.
Also Read:
- Cervical Screening After Vaccination: Why It Still Matters
- Infertility and Laparoscopy: Hope for Couples
Conclusion
Laparoscopy in women’s health is more than just a surgical technique. It represents a shift towards safer, patient-centered care. From defining laparoscopic surgery to exploring diagnostic and therapeutic uses, and weighing benefits against risks, this keyhole operation has transformed gynecology. While not without complications, its advantages of faster recovery, smaller scars, and reduced hospital stays make it a preferred choice for many women.
As a doctor with years of trusted experience, I can assure you that minimally invasive surgery restores confidence, speeds recovery, and transforms women’s health. Book your consultation today to explore if laparoscopy is right for you.
Our Digital Imprints:
Dr. Madhu Goel
Senior Consultant Obstetrician and Gynaecologist
Director, Fortis La Femme
I am passionate about women’s health. With expertise in managing high-risk pregnancies, infertility, and various gynaecological issues, I strive to provide compassionate care. I am committed to ensuring the well-being of my patients. Follow me for insights and updates on women’s health.
Get Connected to my Newsletter
“Health Hub”: Women’s Health & Wellness
Connect with me: Instagram | Facebook | LinkedIn



Good post! We are linking to this particularly great content on our website.
Keep up the good writing.