Cervical Cancer Screening: What Test is Right for You?
Every seven minutes, a woman in India loses her life to cervical cancer—a disease that is both common and largely preventable. The single most powerful step to cut this risk is cervical cancer screening. Unlike many cancers that appear without warning, cervical cancer develops slowly, giving us time to detect and treat changes before they turn dangerous.
As a senior Consultant Obstetrician and Gynaecologist, I have spent over two decades guiding women through preventive care, high-risk pregnancies, and life-saving interventions. Too often, tests are delayed due to fear, discomfort, or lack of awareness.
 This article simplifies the science and shows how timely screening—through a Pap smear test, an HPV test that identifies high-risk HPV, and when needed, a colposcopy procedure—protects your health. You will also find clear cervical screening guidelines tailored to India.
This article simplifies the science and shows how timely screening—through a Pap smear test, an HPV test that identifies high-risk HPV, and when needed, a colposcopy procedure—protects your health. You will also find clear cervical screening guidelines tailored to India.
Ready to explore the right test at the right time and take charge of your cervical health?
Also Read:
Understanding Cervical Cancer and Why Screening Matters
Cervical cancer develops slowly, often over many years. In most cases, cervical cancer begins with a long-lasting infection caused by high-risk types of Human Papillomavirus (HPV).
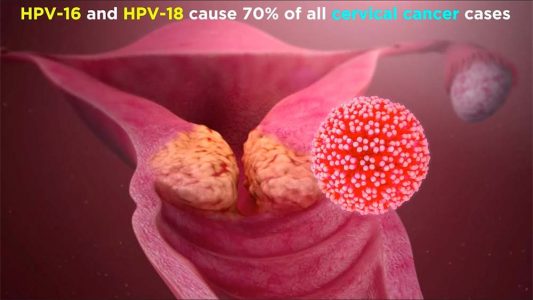 While many HPV infections clear naturally, some types—especially HPV 16 and 18—are responsible for nearly 70 percent of cervical cancers. Without regular checks, these silent infections can cause cell changes in the cervix that progress from minor abnormalities to precancerous lesions and eventually invasive cancer.
While many HPV infections clear naturally, some types—especially HPV 16 and 18—are responsible for nearly 70 percent of cervical cancers. Without regular checks, these silent infections can cause cell changes in the cervix that progress from minor abnormalities to precancerous lesions and eventually invasive cancer.
Key Risk Factors for Cervical Cancer
- Early onset of sexual activity
- Multiple sexual partners
- Smoking and weakened immunity
- History of sexually transmitted infections
- HIV-positive women
As the progression often takes years, timely cervical cancer screening ensures early detection and better outcomes. It detects precancerous changes when treatment is simple and outcomes are excellent. According to cervical screening guidelines, every sexually active woman should undergo routine screening, beginning at age 21.
The Pap Smear Test: A Trusted Standard
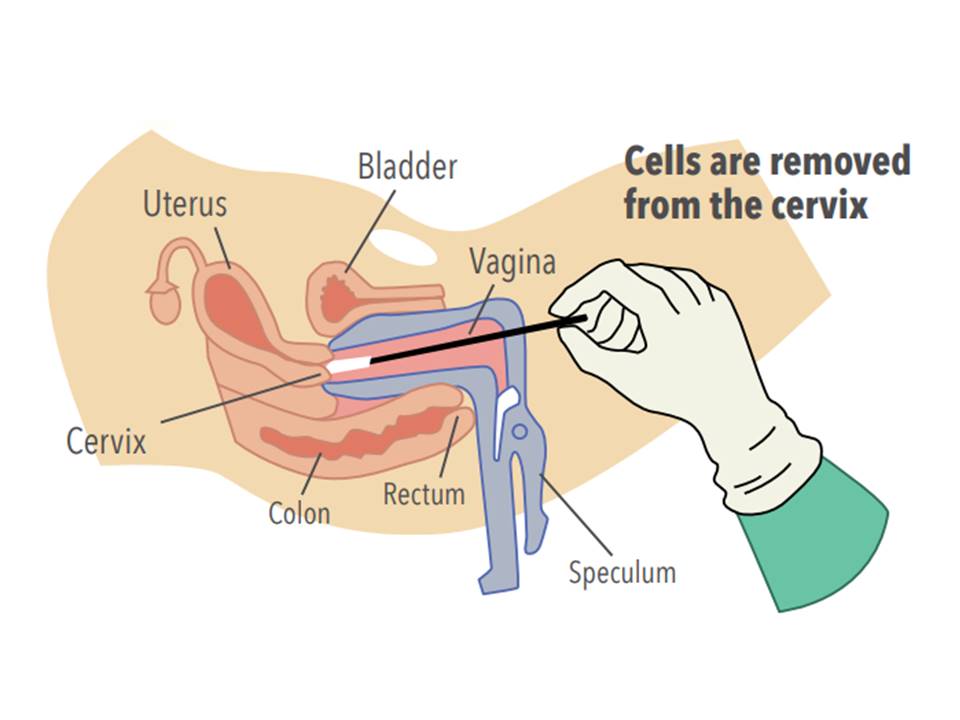
Widely recognized for its role in early detection, the Pap smear test has formed the backbone of cervical cancer screening. It involves gently collecting cells from the cervix with a soft brush or spatula during a pelvic examination. The process is quick, usually painless, and takes only a few minutes. These collected cells are examined under a microscope to detect abnormalities.
Recommended Pap Smear Intervals
- Ages 21–29: every 3 years
- Between 30 and 65 years, women may choose Pap testing every 3 years or combine it with HPV testing once in 5 years.
Advantages of Pap Smear
- Widely available and affordable in India
- Detects abnormal cells before they turn into cancer
- Proven to reduce cervical cancer deaths
Limitations
- May miss some abnormalities (false negatives)
- Needs repeated testing at recommended intervals
While it has its shortcomings, the Pap smear test is still considered an indispensable part of screening. When combined with HPV testing, detection rates improve significantly.
The Role of HPV Test and Co-Testing
The HPV DNA test is a more advanced method, focusing on detecting high-risk HPV types directly. Unlike the Pap smear test, which looks for abnormal cervical cells, the HPV test identifies the virus that causes these changes in the first place. This makes it a more sensitive option for predicting a woman’s future risk of developing cervical cancer. By catching infections before they cause visible abnormalities, it allows doctors to intervene much earlier.
Why HPV Test is Superior
- Detects high-risk HPV strains (especially HPV 16 and 18) years before any cellular changes appear.
- Provides longer reassurance, meaning women with a negative HPV test can safely extend the screening interval.
- Reduces the chances of false negatives compared to Pap smear test alone.
- Helps stratify women into low-risk and high-risk groups, ensuring those who need closer follow-up get it on time.
Research shows that HPV testing identifies almost 95 percent of high-grade precancerous lesions, while Pap smears alone may miss a proportion of these cases. For women aged 30 and above, this reliability is an important breakthrough for preventive care.
WHO Recommendations on HPV Testing
The World Health Organization (WHO) strongly recommends HPV DNA testing as the primary screening method for cervical cancer, especially in countries with high disease burden like India. According to WHO guidelines:
- Women should begin HPV testing from age 30 (or age 25 for women living with HIV).
- HPV DNA testing is preferred over Pap smear where resources allow, because of its higher sensitivity.
- If HPV testing is negative, the next screen can safely be delayed for 5 years, reducing the burden on women and healthcare systems.
- For countries like India, combining HPV testing with awareness and vaccination can dramatically reduce the incidence of cervical cancer.
Co-Testing: Pap Smear + HPV Test
- Recommended for women aged 30–65
- Screening is needed only once in 5 years when results are clear.
- Delivers the most reliable detection of early cervical abnormalities
HPV-Only Screening
Some cervical screening guidelines now permit HPV-only screening every 5 years in women over 30 who have consistently normal results. This strategy is considered safe, effective, and cost-efficient — provided women adhere to follow-up schedules.
Cervical Screening Guidelines in India
Cervical screening in India has traditionally been underutilized, with coverage estimated at less than 5 percent. Yet following national and international guidelines can dramatically reduce the disease burden.
General Recommendations
- Start Pap smear at age 21
- Women 30 years and older should undergo Pap smear combined with HPV testing once every 5 years.
- Women with HIV should start screening earlier (from age 25) and test more frequently
- Screening can stop after age 65 if prior results have been consistently normal
How to Prepare for a Pap Test
- Ideally done on cycle days 8–10
- Do not use creams, douche, or have intercourse 48 hours before testing
- Update your doctor on any medical conditions or recent infections
These practical steps help ensure accurate results and a smoother screening experience.
Taking Charge of Your Cervical Health
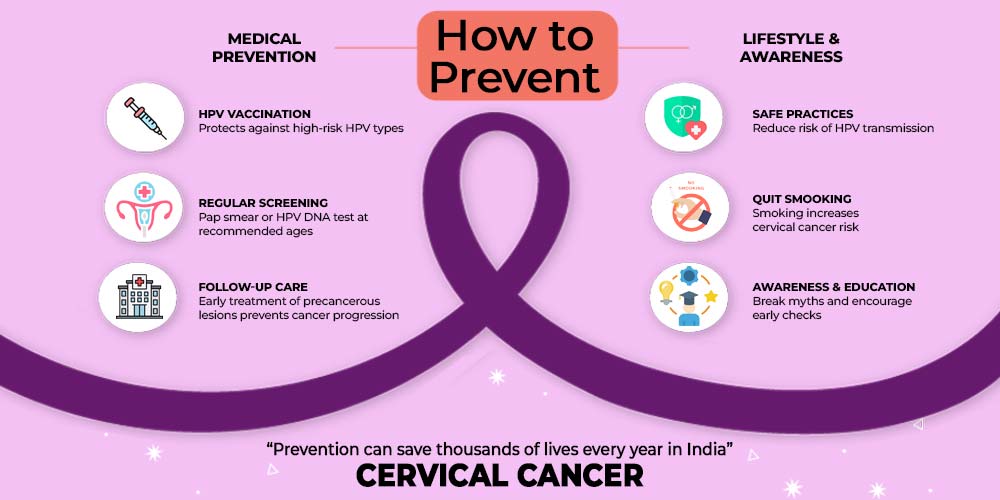
Regular screening together with HPV vaccination offers strong protection against cervical cancer. The HPV vaccine reduces risk by protecting against the most dangerous HPV types, while Pap smear test, HPV test, and colposcopy procedure ensure that any changes are detected early. By following cervical screening guidelines, you can take control of your health and prevent a disease that still claims the life of one woman every seven minutes in India.
Conclusion
Cervical cancer screening is the most effective way to prevent cervical cancer and protect women’s health. Regular Pap smear test, HPV test, and when needed, a colposcopy procedure, allow early detection of high-risk HPV and precancerous lesions. Following cervical screening guidelines in India ensures that women stay protected, even before symptoms appear. Screening combined with HPV vaccination gives the strongest shield against this preventable disease.
As a practising gynaecologist, I urge every woman to take screening seriously and not wait for warning signs. Book your cervical cancer screening today and take charge of your health. To learn more, connect with me, Dr. Madhu Goel, or subscribe to my Health Hub newsletter for trusted insights on women’s health and wellness.
Our Digital Imprints:
Dr. Madhu Goel
Senior Consultant Obstetrician and Gynaecologist
Director, Fortis La Femme
I am passionate about women’s health. With expertise in managing high-risk pregnancies, infertility, and various gynaecological issues, I strive to provide compassionate care. I am committed to ensuring the well-being of my patients. Follow me for insights and updates on women’s health.
Get Connected to my Newsletter
“Health Hub”: Women’s Health & Wellness
Connect with me: Instagram | Facebook | LinkedIn