Recognising the Warning Signs of Ectopic Pregnancy Early
“I had a positive pregnancy test—but something just didn’t feel right.” That’s how many ectopic pregnancy stories begin. No dramatic symptoms. Just a quiet discomfort that’s easy to dismiss—until it becomes dangerous. One such urgent condition is an ectopic pregnancy, where the fertilised egg implants outside the uterus, usually in the fallopian tube. It affects about 1 in 90 pregnancies and can quickly turn life-threatening if not detected early. The challenge? Ectopic pregnancy symptoms often mimic normal early pregnancy signs—making them harder to recognise without awareness.
As a Senior Consultant Obstetrician and Gynaecologist, I’ve seen how early recognition of ectopic pregnancy symptoms can be the difference between a safe recovery and a medical emergency. This article is your guide to understanding the early signs of ectopic pregnancy, how they differ from normal pregnancy symptoms, and when to seek urgent care.
Also Read:
- Ectopic Pregnancy and Fertility: A Guide to Healing, Hope, and Trying Again
- Ectopic Pregnancy: A Complete Patient Guide for Early Detection and Safe Recovery
What Is an Ectopic Pregnancy and Why Is It Dangerous?
In a normal pregnancy, the fertilised egg travels down the fallopian tube and implants in the uterus. But in an ectopic pregnancy, the egg implants elsewhere—most commonly in the fallopian tube (tubal pregnancy), but sometimes in the cervix, ovary, or abdominal cavity.
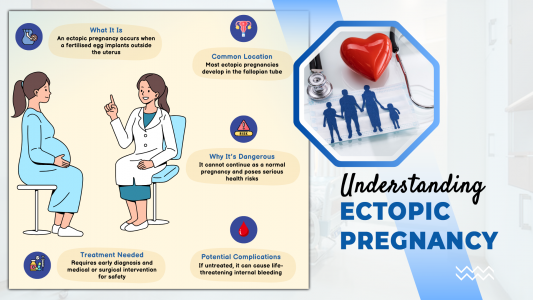
What makes ectopic pregnancy dangerous and why early treatment matters
These areas cannot support a growing embryo. As the tissue expands, it can cause the surrounding structures to rupture, leading to internal bleeding. Without early ectopic pregnancy diagnosis, the condition can become life-threatening. Recognising the signs early is the best way to ensure timely treatment and protect future fertility.
Where Can an Ectopic Pregnancy Occur?
While most ectopic pregnancies develop in the fallopian tube, they can also occur in other locations like the cervix, ovary, or abdominal cavity. This diagram shows how rare sites like interstitial or caesarean scar pregnancies also pose serious risks. Knowing where it can happen helps with quicker diagnosis and targeted care.
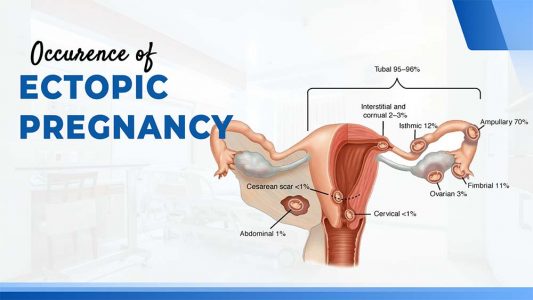
Percentage breakdown of where ectopic pregnancies most commonly occur in the female reproductive system
Ectopic Pregnancy Symptoms to Watch For
Most ectopic pregnancy symptoms appear between the 4th and 10th week of gestation. Unfortunately, these early signs are often mistaken for normal pregnancy discomforts or digestive issues—leading to delayed diagnosis. Recognising these subtle yet dangerous symptoms is crucial.
1️⃣ Missed Period
Often the first sign, it may feel like a typical early pregnancy. But if other unusual symptoms follow, it may signal something more serious.
2️⃣ Sharp Lower Abdominal Pain
Typically one-sided and located in the lower belly. It may feel stabbing, constant, or worsen with movement or urination.

Key warning signs of ectopic pregnancy every woman should know
3️⃣ Vaginal Spotting or Bleeding
Bleeding that’s lighter, darker, or more watery than your period. It may resemble implantation bleeding but persists or becomes heavier.
4️⃣ Shoulder Tip Pain
Caused by internal bleeding irritating the diaphragm. This pain often appears when lying down and is unrelated to arm movement.
5️⃣ Dizziness or Fainting
Triggered by internal bleeding and low blood pressure. May be paired with confusion or nausea.
6️⃣ Pain During Urination or Bowel Movements
Unusual discomfort when passing urine or stools could indicate internal pelvic irritation.
If you experience any combination of these symptoms—especially with a positive pregnancy test—don’t wait. Seek immediate medical attention. Early recognition of ectopic pregnancy saves lives.
Ectopic Pregnancy Pain vs Normal Pregnancy Cramping
It’s common to feel cramping in early pregnancy, but not all pain is harmless. Understanding how ectopic pregnancy pain differs from typical pregnancy discomfort can help you take timely action—and avoid dangerous complications.
| Symptom | Normal Pregnancy | Ectopic Pregnancy |
| Mild cramping | Common, central in lower belly | Sharp, localised, worsening with time |
| Spotting or light bleeding | Normal during implantation | Irregular, darker, prolonged spotting |
| Nausea and vomiting | Morning sickness | Often paired with pain or dizziness |
| Shoulder tip pain | Not expected | Serious sign of internal bleeding |
| Dizziness or fainting | Unusual | Urgent warning of tubal rupture |
This table is not just a reference—it’s a life-saving comparison. If your symptoms feel unusually sharp, intense, or just not right, trust your instincts—your body may be signalling a serious concern.
When to Seek Medical Help in Pregnancy
Seek urgent medical care if you experience any of the following:
- Sudden, severe one-sided abdominal pain that doesn’t go away
- Heavy bleeding or unusual spotting in early pregnancy
- Shoulder tip pain, especially when lying down or taking a deep breath
- Faintness, dizziness, or a rapid heartbeat
- Extreme weakness, confusion, or feeling like you might collapse
Even if you feel unsure, it’s better to get checked. A transvaginal ultrasound and serial hCG tests are the standard tools for ectopic pregnancy diagnosis. These tests confirm whether the pregnancy is inside the uterus and progressing as expected.
The Role of Awareness in Ectopic Pregnancy Diagnosis
The biggest challenge? Many women don’t experience noticeable symptoms until the ectopic pregnancy has already ruptured—making early detection even more critical. That’s why awareness—both among patients and providers—is crucial. Educating women about early signs of ectopic pregnancy should be part of every prenatal care program.
Women undergoing fertility treatments, those with a history of PID, previous ectopic pregnancy, or tubal surgeries are at higher risk. If you fall into one of these groups, early ultrasound (around 5–6 weeks) is strongly advised.
What Happens If You’re Diagnosed with an Ectopic Pregnancy?
Once ectopic pregnancy diagnosis is confirmed, the only safe option is to end the abnormal pregnancy—because it cannot progress normally and poses serious risks. Treatment depends on how early it’s detected and your overall condition.
- Methotrexate Injection: A medication that stops the growth of the ectopic tissue if caught early and the tube hasn’t ruptured.
- Laparoscopic Surgery: A minimally invasive procedure to remove the ectopic pregnancy. The affected fallopian tube may also be removed if it is ruptured or severely damaged.
- Laparotomy: Emergency open surgery if internal bleeding is life-threatening.
With early diagnosis, recovery is quicker, and future fertility can be preserved.
Also Read:
Final Thoughts: You Know Your Body Best
An ectopic pregnancy is not your fault. But not recognising the warning signs could cost you your health—or your life. A good healthy diet is about providing the building blocks for quick recovery.
You don’t have to wait for unbearable pain or collapse to act. If you suspect anything unusual, speak to your doctor immediately. At my clinic, we prioritise early detection, evidence-based care, and emotional support for every patient.
Let’s make Ectopic Pregnancy Awareness Month a time to spread knowledge, offer support, and encourage every woman to trust her instincts.
📌 Takeaway Checklist
- Recognise the early signs of ectopic pregnancy—even if they seem mild
- Pay attention to sharp one-sided abdominal pain and unusual vaginal bleeding in early pregnancy
- Don’t ignore shoulder pain or dizziness
- Seek urgent care incase your pregnancy test is positive
- Get a transvaginal ultrasound and serial hCG levels checked early
Our Digital Imprints:
Dr. Madhu Goel
Senior Consultant Obstetrician and Gynaecologist
Director, Fortis La Femme
I am passionate about women’s health. With expertise in managing high-risk pregnancies, infertility, and various gynaecological issues, I strive to provide compassionate care. I am committed to ensuring the well-being of my patients. Follow me for insights and updates on women’s health.
Get Connected to my Newsletter
“Health Hub”: Women’s Health & Wellness
Connect with me: Instagram | Facebook | LinkedIn